Home » Dry Eye
People are often unaware that there are effective treatments for dry eye. If you struggle with uncomfortable or debilitating dry eye symptoms and want relief, turn to Sun Laser Vision Center. Our team of eye-care experts are here to guide you to the best treatment among the many different options available for dry eye. These treatments can reduce unpleasant symptoms, improve your vision performance and reduce your risk of developing complications. Call the office to schedule an appointment.
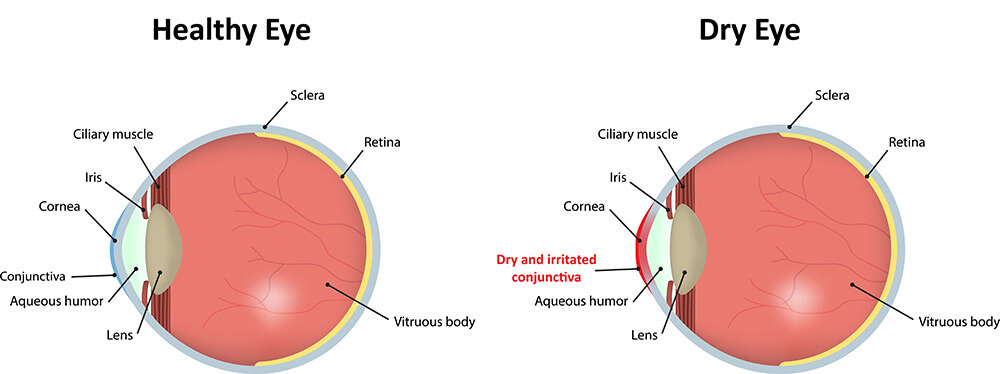
What is Dry Eye?
Dry eye is a condition that reduces production of healthy tears which protect your eyes and focus your vision. It can make your eyes feel very uncomfortable and indicate an underlying problem that needs to be treated. Because dry eye is very common in our desert community it is an area that the eye-care experts at Sun Laser Vision Center are passionate about treating.
What Are the Symptoms of Dry Eye?
Dry eye can cause the following symptoms:
- Dryness
- Redness
- Burning
- Irritation
- Gritty sensation
- Periods of dryness followed by excessive tearing
- Blurry vision
- Eye tenderness
What Are the Risk Factors for Dry Eye?
Dry eye can affect anyone, but some things increase your risk of developing it, including:
- Older age
- Female gender
- Genetics
- Hormone changes
- Some medications
- Certain medical problems
- Environmental and work conditions
Examples of medical conditions that can cause dry eye include rheumatoid arthritis, lupus, Sjögren’s syndrome, scleroderma, thyroid problems, and diabetes. If someone in your family has dry eye, you’re more likely to experience the condition yourself.
How Does My Eye Doctor Diagnose Dry Eye?
To find out if you have dry eye and develop an effective treatment, your ophthalmologist discusses your medical history and symptoms and completes a thorough eye exam. Tests measure the sodium level in your tear’s film and the overall quality of your tears.
Click the button below to request an appointment today.
LEARN MOREHow is Dry Eye Treated?
Common treatments for dry eye include:
- Intense pulsed light (IPL)
- Thermal treatment of the eyelids
- Punctal plugs
- Artificial tears
- Eye medications
- Eyelid hygiene
- Moist heat-releasing dry eye masks
These treatments are usually painless and non-invasive, but they can offer good results. They can improve your tear production, reduce irritation, improve comfort and your quality of life.
Your treatment is personalized to your particular set of issues to try to be the most effective in relieving your symptoms. We monitor your progress and make changes to your treatment as needed.
There are effective treatments for dry eye. Don’t live with uncomfortable dry eyes when you don’t have to.
Treatment for Dry Eye
There are now many treatment options available for patients with chronic dry eye. This can include multiple medications designed to improve tear production. There is a new nasal spray to help as well as a silicone plug that can be placed in the lower tear drain in the eyelid to retain more moisture. Treatments for eyelid problems that can contribute to dry eye are also available. Tailoring the individual options to best suit your needs is important to help you get the best results. Call us to learn more about the options available to you.
Schedule an appointment today with Sun Laser Vision Center.